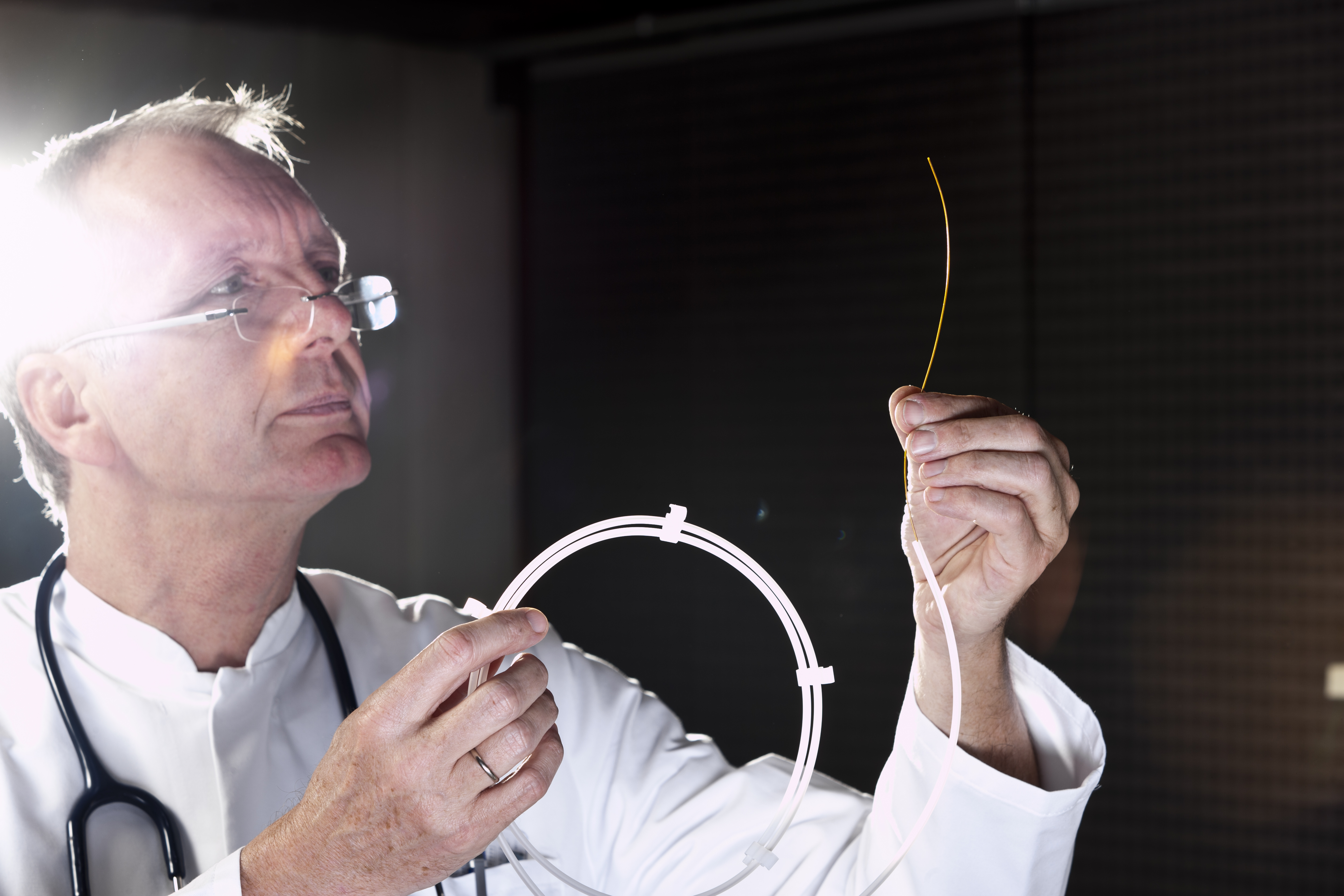
Whether you’ve just had surgery or are suffering from an illness or injury, when your ability to urinate becomes compromised, catheterization is often necessary. Using a catheter lets you live as normally as possible – but finding the right catheter isn’t an easy task.
Today, there’s a wide array of catheters available. If you need catheterization for the short- or long-term, you need to find the right catheter. And the only way to do so is with research into the available options.
 Types of Catheters
Types of Catheters
When a catheter becomes a necessity, you’ll quickly find out why it pays to select the right one. Although catheters are generally safe and easy to use, they can cause problems if the wrong one is used or if a catheter is used incorrectly.
There are four primary types of catheters you can choose from:
1. Indwelling Catheters
An indwelling catheter is one that’s placed in and stays in the bladder. When inserted through the urethra, this type of catheter is known as a Foley catheter; when inserted through a tiny hole made in the abdomen, which may be done when the urethra is blocked or damaged, it’s known as a suprapubic catheter. After insertion, a tiny balloon at the end of the catheter is filled with water to keep it in place.
Indwelling catheters are typically best for people who are unable to urinate on their own because of illness or injury. Conditions that may warrant the use of an indwelling catheter include an excessively enlarged prostate; blood clots in the urine; and blocked flow because of kidney or bladder stones.
2. Intermittent Catheters
If you’re capable of urinating naturally, an intermittent catheter is generally the preferred way to go. Safe for short-, mid- and long-term usage, intermittent catheters are inserted just until the bladder is emptied.
Also known as “in and out” catheters because of how they’re used, intermittent catheters are commonly used after surgery. They’re also often prescribed for people who suffer from urinary retention, which means the inability to completely empty the bladder; this condition affects approximately 4.5 to 6.8 out of every 1,000 men according to the National Association for Incontinence¹.
3. Hydrophilic Catheters
Hydrophilic catheters feature a sterile saline lubrication that’s activated with water. This eliminates the need to use a separate lubricant when applying the intermittent catheter, so it saves time and effort. It also reduces the risk of irritation, which can be an ongoing problem with other catheter types. Most hydrophilic catheters are designed for one-time use.
4. Non-Hydrophilic Catheters
Non-hydrophilic catheters must be lubricated separately, but they can be cleaned, sterilized, and used several more times. For people who rely on catheters for extended periods of time, non-hydrophilic catheters often make the most sense. They’re also optimal for people who have sensitivities to the lubricants used on hydrophilic catheters.
Does Medicare Cover Catheters?
Medical care of any kind isn’t cheap, and it’s normal to be concerned about the ongoing costs associated with catheters. No matter the catheter you use, the cost of these supplies can add up quickly — and that’s especially true for people on fixed incomes.
Luckily, Medicare covers the cost of catheters and related supplies for many situations. According to Aero Flow Urology², as long as a doctor has deemed catheters to be medically necessary, you can expect for the devices and related supplies to be covered by your Medicare plan.
\Medicare may cover catheters following surgery if they’re prescribed by your doctor and deemed to be medically necessary for your recovery. If you undergo outpatient surgery that requires catheterization afterwards, you can expect Medicare Part B, the medical insurance part of Medicare, to cover it; if you undergo inpatient surgery that requires catheterization, you can expect Medicare Part A, the hospital insurance part of Medicare, to cover it.
If your doctor prescribes catheterization to address urinary retention or urinary incontinence, the catheters may be covered by Medicare if they will be needed for at least three months or permanently. Whether Medicare covers catheters following surgery or for urinary incontinence or retention, a Medicare Supplement plan, which is also known as Medigap, may be used to cover all or part of out-of-pocket expenses like coinsurance, copayments and deductibles. This could save you considerable money over the long haul.
Finally, Medicare may also cover some or all the supplies that are associated with catherization, and this can help immensely with affordability. You must rely on many tools when using catheters, and they can start to get very expensive over time. Depending on why you have been prescribed a catheter, your Medicare plan may cover related supplies like extension tubing; bedside drain bags; leg bags; irrigation kits and irrigation syringes.
Although relying on a catheter isn’t a walk in the park, modern devices are safe and easy for pretty much anyone to use. If you will need a catheter either for the long- or the short-term, do some research to determine which type makes the most sense for you — and confirm what is and isn’t covered by your Medicare plan to avoid unpleasant surprises.


